More than 12 million Americans with Medicare also have Medicaid. These “dual-eligibles” typically have few out-of-pocket health care costs, whether they are in Traditional Medicare or a Medicare Advantage plan. Still, the Kaiser Family Foundation reports that half of them choose a Medicare Advantage plan, even though Medicare Advantage restricts their access to health care providers and imposes other barriers to care.
People with Medicare and Medicaid, “dual-eligibles,” can get coverage through Traditional Medicare, with Medicaid picking up deductibles and coinsurance costs, through standard Medicare Advantage plans, or through Medicare Advantage plans designed specifically for dual-eligibles. Because there is so much we don’t know about Medicare Advantage plans, including denial rates and wait times for coverage, much less how quality differs among these plans, dual-eligibles should be better off in Traditional Medicare, where it is far easier to get care than in a Medicare Advantage plan.
In the ideal world, health systems would do a good job of coordinating people’s care. But, that’s not the world we live in. Still, a lot of people with Medicare and Medicaid opt for a Medicare Advantage plan. Misleading ads and sales agents can be convincing.
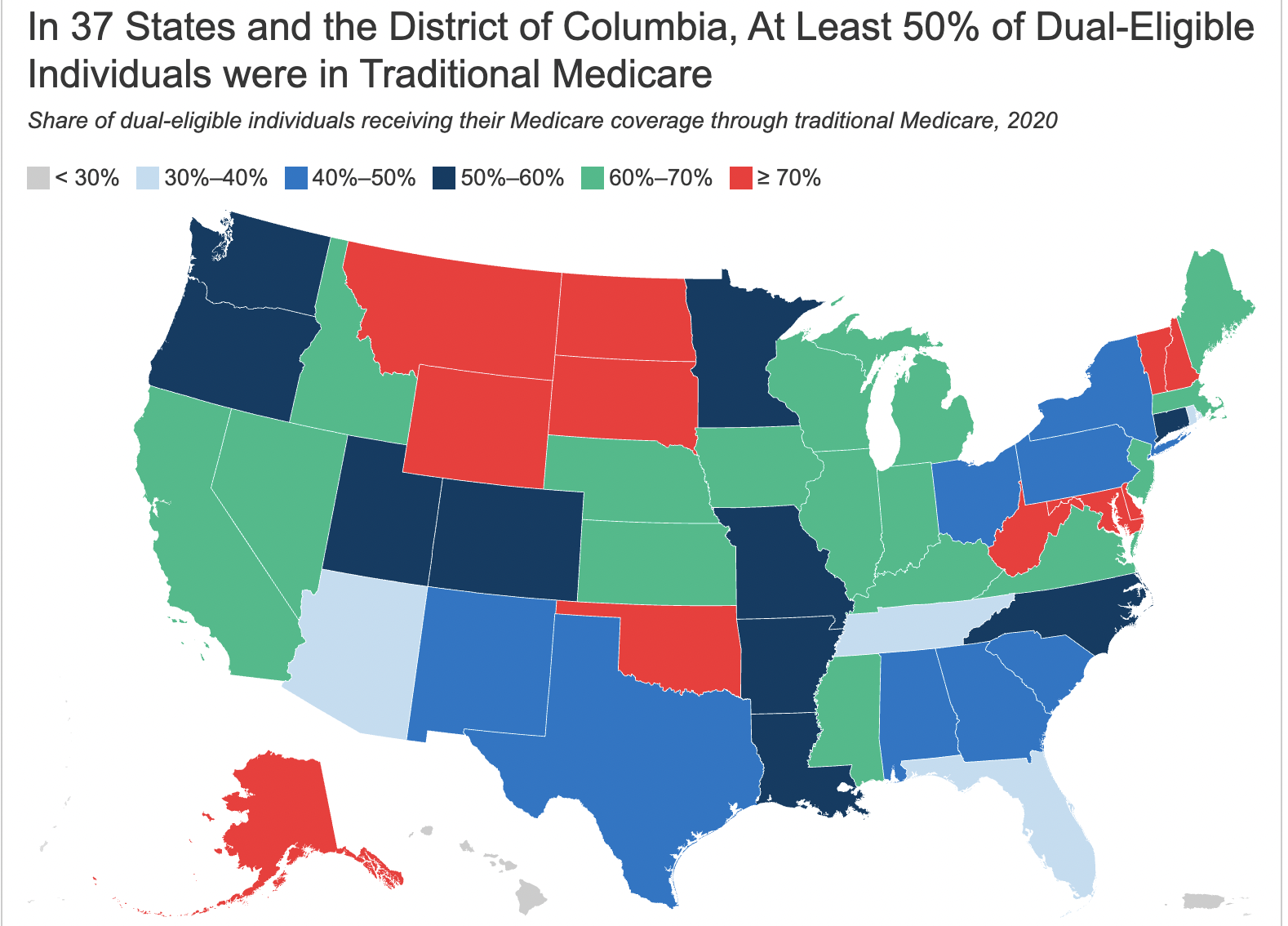
About half of dual-eligibles are enrolled in corporate-run Medicare Advantage plans when they would likely have easier access to care in Traditional Medicare. Traditional Medicare covers your care from almost all health care providers in the US without prior authorization requirements. Black, Hispanic and Asian/Pacific Islanders are more likely to sign up for Medicare Advantage plans than non-Hispanic White people.
About three in ten dual eligibles are enrolled in Medicare Advantage Special Needs Plans or SNPs, which are corporate health plans intended to coordinate their care and to work well with Medicaid in their states. But, it’s not clear how well these plans work. In fact, the Office of the Inspector General recently released a report expressing concerns about high inappropriate denial rates in some Medicaid health plans.
One great Medicare program that coordinates care for dual-eligibles is PACE, the Program of All-Inclusive Care for the Elderly. If you are a dual-eligible, look into the non-profit PACE programs in your area. They are often unable to take new enrollees, but if you can get on a waitlist, do so. To qualify for the medical and social services they provide, you must be at least 55 years old and be able to live in your home safely but need a nursing home level of care. For more information on PACE, click here. Note: Beware of for-profit PACE programs.
Here’s more from Just Care:
- PACE helps older adults stay in their community
- For-profit PACE programs: Cause for worry?
- Office of Inspector General finds insurers inappropriately deny care to people with Medicaid
- Six tips for keeping your drug costs down if you have Medicare
- What are your Medicare premium and other costs in 2023?
Leave a Reply