In the fourth article of a multipart series on health literacy and innovation in health care...
Drugs and technology
Pharma’s role in our opioid crisis
By some accounts, 2.6 millions Americans are addicted to painkiller...
Health tech–A primer
What is the Internet of Things exactly or the Quantified Self? And, is it really important for you...
FAIR Act would force drug makers to justify big price hikes
A bi-partisan group of Senators and Representatives, led by Tammy Baldwin and John McCain...
Pharma pushing states to cover high-cost drugs
When it comes to drug innovations, many would argue that pharmaceutical companies serve the public...
Drug companies must now disclose most clinical trial results
For years, drug and medical device companies have been able to conduct clinical trials and then...
Why should drug companies have extra monopolies?
In a Health Affairs article, Alfred Engelberg explains that over the course of the last 35...
Risk to older adults of underuse of prescription drugs
A paper in the British Journal of Clinical Pharmacology reports on the risks of underuse of...
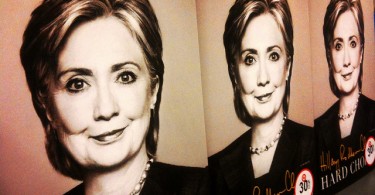
Clinton proposes plan to rein in some drug prices
Recognizing that government intervention is needed to rein in some drug prices, Hillary Clinton has...
Facts about prescription drug prices in the U.S.
The High Cost of Prescription Drugs in the United States, a new JAMA paper by Aaron Kesselheim, MD...