As we age, it is all too common to think that we are beginning to suffer from dementia. Please be assured that small memory lapses are not signs of dementia. What are the symptoms? Dementia is...
Emily Shearer
Six reasons why you and your loved ones should create advance...
Advance care planning is important for your peace of mind and for the people you love. You should begin care planning by creating an advance directive. An advance directive is a legal document that...
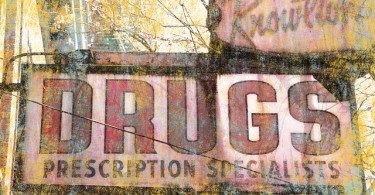
Six things to know about your over-the-counter medications
Over-the-counter medications are drugs you can buy without a prescription to treat common problems. However, you should still use them with caution. A number of recent studies have revealed...
Living well with dementia: The benefits of early diagnosis
Are you concerned that you or someone you love is showing signs of dementia? If so, the benefits of early diagnosis of dementia are significant. There are some treatments for dementia, including...
How to prepare for your hospital stay
Going to the hospital for an overnight stay, whether it is for a scheduled surgery or for medical tests, can cause irritation, stress, and even anxiety. Knowing how to prepare for your stay can...
The Five ‘Rights’ Rule for Taking Medications
We all know that both prescription drugs and over-the-counter medications can help keep us healthy. But, it is estimated that 50 percent of people do not comply with their medication...