Elderly nursing home patients prescribed a multitude of medications following a heart attack may live longer compared to those given just one prescription drug, but it can come at a cost: It may...
Jonathan Block
PPIs found to increase risk of kidney failure
Routine use of proton pump inhibitors, common over-the-counter medications used to treat acid reflux, can increase the risk of kidney failure four-fold. Researchers examined health data on more than...
More men at low risk for prostate cancer wait and see about...
An increasing number of men at low risk of developing prostate cancer are choosing a wait-and-see approach in lieu of treatment options such as radiation or surgery. In 2010, 14.5% of men with...
Do you really need that antibiotic?
According to a new study in BMJ, nearly one-quarter of antibiotic prescriptions filled by those with private insurance were not medically justified, leading to concerns about antibiotic overuse...
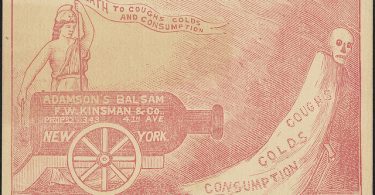
Talk to your doctor before taking a cold medicine
With cold and flu season in full swing, people with high blood pressure that is not controlled well or who have heart disease need to be careful with over-the-counter cold medicines, as they may...
Higher risk of car accidents for people on multiple meds
While it’s no surprise that many older adults take a lot of different medications, many of those drugs can potentially increase their risk of getting into an automobile accident. A new...
If you take supplements, beware of potentially serious...
Millions of seniors that take herbal supplements in addition to prescription drugs may be at risk for potentially serious supplement-drug interactions. Researchers in the UK polled older adults 65...
Don’t overlook marijuana-prescription drug interactions
Middle-aged and older adults are increasingly using marijuana. As these groups tend to take more medications, marijuana-drug interactions are overlooked. When I think of a typical marijuana user, I...
Aspirin may not help to prevent heart problems
People who are at a moderate risk of developing cardiovascular disease who take a low-dose aspirin daily do not have fewer heart problems compared to those who don’t take anything, according to a...
At-home cancer test is largely unhelpful
If you could take a test and have it determine whether you are at an elevated risk for developing breast cancer, who wouldn’t want to know such valuable information? And what if you could do it in...