Until recently, the Medicare Part B premium (medical insurance) was the same for everyone...
Your Coverage Options
If your doctor leaves your Medicare Advantage plan mid-year, you...
There are reasons you should not trust your health plan’s provider directory, and you can...
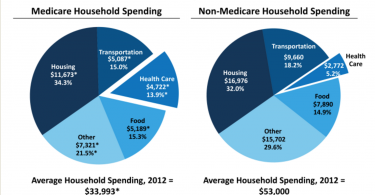
People with Medicare spend significantly more on health care...
Many people do not realize that health care costs are almost 14% of household income for people...
Three reasons why you can’t choose a health plan...
If you’re struggling to choose a health plan that’s “right for you,” you’re in...
The price you pay for a narrow network
These days, choosing a health plan that saves you money is a bit like throwing a dart. If you...
Don’t let your doctor intimidate you: A personal story
It was a balmy fall day last year, when I walked through the surprisingly creaky door of a...
Medicare covers depression screenings
Depression can be crippling, disrupting people’s daily lives and normal functioning. But it...
Health plan networks limit access to care
One of the biggest problems with health insurance companies is that they generally offer health...
Observation care: What you need to know
For the last couple of decades, instead of admitting all Medicare patients who stay overnight as...
Can you budget for your health care?
If you have commercial health insurance, be it a Medicare Advantage plan, a state health exchange...