Because the Supreme Court gave states the option of expanding Medicaid, it has forced about four...
Your Coverage Options
How safe are outpatient surgery centers?
Medicare now covers surgeries in some 5,500 outpatient surgical centers. Patients often like...
Benefits and risks of telemedicine
Telemedicine allows doctors to remotely assess the conditions of patients via telephone or video...
Pneumonia vaccine: Medicare covers it
You should do what you can to avoid getting pneumonia, especially if you’re older. Pneumonia is a...
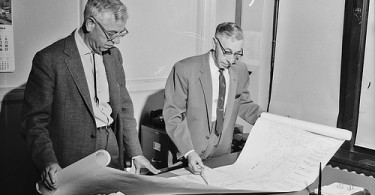
Three big differences between a private Medicare fee-for-service...
Today, just as 50 years ago, when President Johnson signed Medicare into law, traditional Medicare...
If your Medicare drug plan refuses to cover your medications...
Too often, pharmacists are unable to fill prescriptions for people with Medicare because their Part...
Medicare proposes to pay for advance care planning
In a newly released proposed rule, Medicare is proposing to pay for individuals to talk to their...
Respite care: Medicare may pay for you to take a break when...
It can be very stressful as well as physically demanding to take care of anyone, particularly...
ER visits for dental care on the rise, but some states are...
Data from the American Dental Association reveals that emergency room visits for dental care more...
Eight things you should know about the Affordable Care Act
Thanks to the Affordable Care Act (“ACA”), 16.4 million more people in the United States have...