Kaiser Health News reports on a ghastly phenomenon that appears all too common for people with...
Medicaid
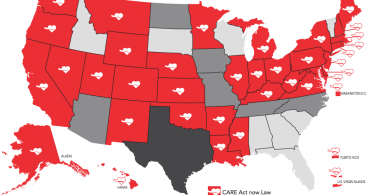
CARE Act assists family caregivers
About seven in ten older adults need long-term care at some point. In many cases, it is a family...
Before choosing a nursing home, check out Nursing Home Inspect
If you are looking into nursing home options, Pro Publica has an online tool worth exploring...
Protect your eyesight: Free and low-cost vision care
Your ability to see well is precious. But, your vision is likely to deteriorate as you age. Some...
Free and low-cost ways to address hearing loss
While our hearing is likely to weaken with age, there are things we can do to address hearing...
How to get free or low-cost dental care
Because dental care can be so expensive and most insurance—including Medicare—does not cover...
Are commercial Medicaid and Medicare plans a good taxpayer...
How do we know whether commercial Medicare and Medicaid health plans are a good taxpayer...
Congress must protect our community health centers
Every Thursday morning, I wake up excited for the 14-hour day I’m about to begin. My Thursdays...
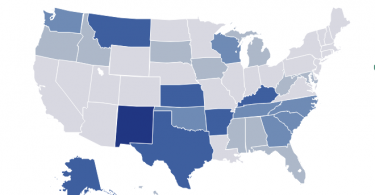
Medicaid: Why it matters to all of us
Medicaid, with “aid” at the end, is a federal-state insurance program established to help...
ACA reduces medical divorces
Among the Affordable Care Act’s many benefits, it’s common knowledge that it has...