Medicare Open Enrollment begins on October 15 and runs through December 7. During this time...
Medicare
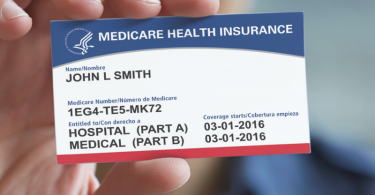
New Medicare card in the works
The Centers for Medicare and Medicaid Services, CMS, is preparing to release a new Medicare card to...
2018 Social Security benefits should rise, but checks may not
One of the strengths of Social Security is that benefits are adjusted annually to offset increases...
What are Accountable Care Organizations?
Medicare has been experimenting with new payment models to bring down health care costs, improve...
What to do if your in-network doctor goes out of network?
It used to be that our health care system valued continuity of care. Insurers covered care from...
Three things to consider about end-of-life care
If you’re caring for someone at the end of life–with a life expectancy of no longer...
No projected 2018 increase in standard Medicare premium
[Editor’s note: Medicare 2018 premium information released, November 20, 2017.] The July...
Medicare should cover dental, vision and hearing services
A new paper in JAMA, by Amber Willink, Cathy Schoen and Karen Davis, explains why Medicare should...
How to protect yourself against unexpected medical bills
If you’ve been to the hospital at any time in the last several years–be it for a scheduled...
Mental health telemedicine growing in rural areas
At both the federal and state levels, there is a growing interest in telemedicine. But how is it...