Earlier this month, MedPAC, the agency that oversees Medicare payments, released a slide deck showing ever-increasing government overpayments to Medicare Advantage plans.The total overpayments stemming from “upcoding,” additional diagnoses codes on patient records, are staggering, while concerns about quality of care remain. Will the administration and Congress stop the billions in overpayments and protect Medicare Advantage enrollees from health plans that are keeping people from getting needed care?
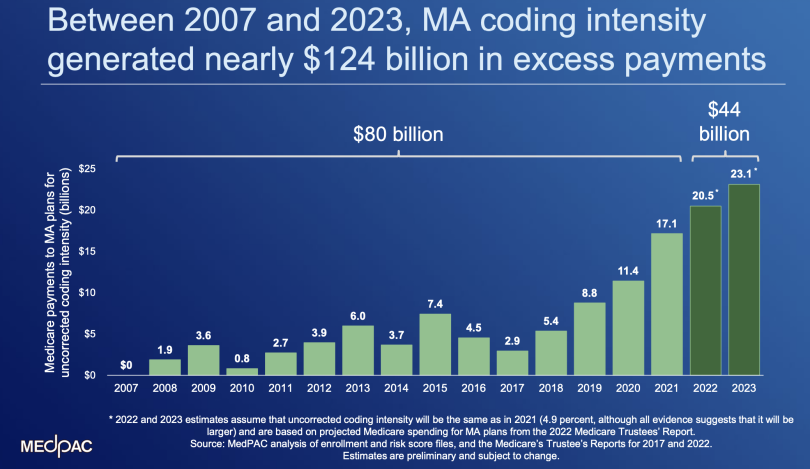
The overpayments that are the focus on MedPAC attention amount to more than $124 billion between 2007 and 2023. They stem from Medicare Advantage plans adding diagnosis codes to patient charts, as currently permitted. They are different from the overpayments from wrongful or fraudulent diagnosis codes.
With each passing year, Medicare Advantage likely will grow, as will the permissible government overpayments to Medicare Advantage plans, unless things change. This year and last alone, according to MedPAC, overpayments totaled $44 billion, $17 billion in 2022 and $27 billion in 2023. Take a look at the chart accompanying this post.
These permissible overpayments are so high that people in Medicare Advantage plans theoretically have $2,350 in additional benefits each year. But, there is no evidence they do. They most likely end up in the coffers of Medicare Advantage plans. People in Medicare Advantage needing costly care continue to face widespread and persistent delays and denials of care, jeopardizing their health. MedPAC also expressed ongoing concerns about quality of care in Medicare Advantage.
These Medicare Advantage overpayments are projected to total more than $600 billion in the next eight years. Over time, these additional payments will likely come back to haunt Medicare Advantage enrollees. They will probably face much higher out-of-pocket costs.
Congress and the administration eventually will change the Medicare Advantage payment system to eliminate these overpayments. If they don’t, the cost of Medicare Advantage, which insurers argued back in 2003 would be 90 percent of Traditional Medicare, will become unsustainable. The government is currently spending 106 percent of Traditional Medicare on Medicare Advantage.
What will happen to people with Medicare when Congress changes the Medicare Advantage payment system? If they’re in Medicare Advantage, most will be locked in, unable to switch to Traditional Medicare, and will have to pay significantly higher costs. Congress has opted not to have an out-of-pocket cap in Traditional Medicare nor has it given people a guaranteed right to supplemental coverage in Traditional Medicare so they can protect themselves from financial risk. What a big f#$%ing mess.
Here’s more from Just Care:
- The high costs of Medicare Advantage and how to address them
- OIG finds widespread inappropriate care denials in Medicare Advantage
- CMS overpays Medicare Advantage plans and lets them keep the extra billions
- Congress must overhaul the way it pays Medicare Advantage plans
- Four things to think about when choosing between traditional Medicare and Medicare Advantage plans