A new report by the Association of American Medical Colleges (AAMC) projects a doctor shortage over the next ten years of between 61,700 and 94,700, with a primary care doctor shortage of between 15,000 and 35,600. To address the doctor shortage, AAMC recommends a multi-pronged approach, including federal support of 15,000 more residency positions over the next five years as well as support for new care-delivery models and technologies.
The rise in demand for doctors stems largely from a projected 41 percent increase in the number of people over 65 in the next ten years. The projected shortfall in doctors results as well from the fact that more than one in three doctors will be over 65 in 2025 and many will retire. Today, about 37 percent of doctors are between 55 and 75. The impact of the Affordable Care Act and the higher number of insured Americans on the doctor shortage is less than expected at 1.2 percent.
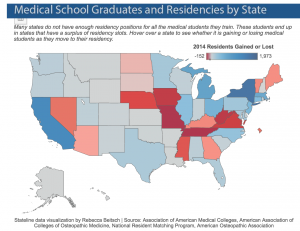
Currently, medical schools are expanding their classes to enroll more students, but these students often struggle to find residency programs. The federal government caps enrollment in residency positions, limiting access. Under the Balanced Budget Act of 1997, Medicare cannot spend more than $9.5 billion a year on residency programs, and it is the largest funder of these programs.
In the last 20 years, there are 20 more medical schools–175 total–and hundreds more students graduating from them. Five hundred students could not secure residencies in 2013. Many residency programs and states are taking matters into their own hands, finding money to increase residency slots. But, that is no small feat since each slot is estimated to cost $150,000.
At the same time, there is a need to ensure that more doctors deliver primary care. Yet, the percentage of doctors going into primary care is lower than ever before. The cost of medical schools and residency programs drives doctors into specialty care that helps ensure that they can pay off loans. Thousands of prospective doctors are drowning in debt. The National Health Service Corps and other loan repayment programs can encourage doctors to enter primary care medicine and to practice in underserved communities.
To be sure, addressing doctor shortfalls in underserved communities presents a challenge; it likely means establishing more residency slots in these communities. One study found that only 48 of more than 1,390 residency programs and training sites in family medicine (4 percent) and only 48 of 936 in internal medicine (5 percent) are in rural or community-based settings. Exposure to these settings is more likely to lead doctors to practice in these settings, so the researchers recommend more residency programs in these settings.
Congressmen Joseph Crowley (D-NY) and Charles Boustany, Jr., M.D. (R-LA) have introduced H.R. 2124 the Resident Physician Shortage Reduction Act of 2015, which supports 3,000 more Medicare direct graduate medical education and indirect medical education residency positions each year for five years beginning in 2017.
Here’s more from Just Care: