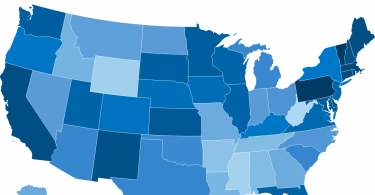
The Delta variant of the novel coronavirus is wreaking havoc in the US because so many Americans...
Uncategorized
Profit motive among hospitals and group practices poses huge...
This post was originally published on the Health Justice Monitor. Recent Changes in Physician...
How to avoid food poisoning
Consumer Reports explains that food poisoning comes from sources other than food. So, you might...
Why does private health insurance work well in Europe?
Many Americans wonder why private health insurance works to guarantee people good affordable care...
Does coffee, tea or chocolate improve your brain’s health
You may have read that the different phytochemicals in fruits can be good for your health...
Lifting weights may help you think better
The New York Times reports that a new study published in the Journal of Applied Physiology shows...
Higher risk of car accidents for people on multiple meds
While it’s no surprise that many older adults take a lot of different medications, many of those...
What is wrong with Medicare prices for all?
In the latest issue of the Washington Monthly, Paul Hewitt and Phillip Longman make the case for...
Long-term care at a glance; many of us will need it
Because we don’t live forever, it’s important to be prepared in the event that you or a loved...
What to do if your in-network doctor goes out of network?
It used to be that our health care system valued continuity of care. Insurers covered care from...