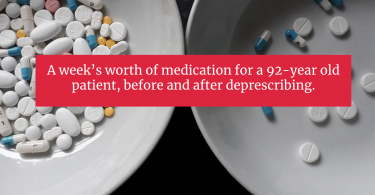
Should you be taking all the medications you are taking? With medicine, sometimes less is more. ...
Drugs and alcohol
Coronavirus: Why are older adults most at risk?
You might be wondering why it is that older adults are most likely to be at risk if they get...
Drug prices: It’s time for the federal government to step...
Fran Quigley writes for Common Dreams about the need to end pharmaceutical company monopolies if...
Warning: Your hip replacement could kill you
Jeanne Lenzer writes for the New York Times about the danger of getting a hip replacement. In some...
One in seven older adults experience harmful drug side effects
More than nine in ten older adults take at least one prescription drug; And, half of all older...
Should you be drinking grapefruit juice?
Grapefruit juice, which is filled with vitamin C and potassium, can be part of a healthy diet...
One pharmacy uncovers dangerous chemicals in some common drugs
A small pharmacy based in New Haven is testing the prescription drugs it dispenses for safety. And...
Dangerous side effects from anticholinergic drugs
Judith Graham reports for Kaiser Health News on frequently used over-the-counter and prescription...
Opioids can kill you
We all know the pleasures of a good painkiller. We often don’t know the risks. If...
Before ordering generic drugs from Canada or any other country...
If you’re one of the millions of Americans who has bought lower-cost medication from Canada or...